Reimbursement Rates Explained How Much Will You Get Back
The text discusses the definition and factors of healthcare reimbursement rates, the calculation of reimbursement rates and factors, different reimbursement methods and formulas, helpful tips for negotiating and maximizing reimbursement rates, and a section detailing how to ensure you are maximizing your reimbursement rates.
Key Takeaways:
Understanding Reimbursement Rates
Understanding reimbursement rates is essential for both companies and employees as they form the basis for reimbursing business expenses. Companies must establish fair and compliant reimbursement rates to ensure employees are fully reimbursed for their expenses.
Accurate rates are crucial for organizations to comply with federal tax laws, helping to prevent audits and penalties resulting from incorrect expense reporting. Fluctuations in reimbursement rates can impact a business’s financial health, affecting profitability and budgeting.
Fair reimbursement rates are important for employees not only for financial compensation but also for enhancing job satisfaction and morale. Different types of expenses may require varying rates based on insurance policies and industry standards, necessitating careful consideration and calculation of reimbursement structures.
Definition and Explanation
Reimbursement is the process through which healthcare providers receive payment from insurance companies for medical services rendered. It plays a critical role in enabling quality medical service providers to sustain the delivery of care to patients.
Different reimbursement models, such as fee-for-service, capitation, and value-based care, have varying implications for both providers and patients. Health insurance serves as an intermediary facilitating reimbursement by coordinating payments between providers and insurers. The type of health insurance policy a patient holds can impact reimbursement rates and out-of-pocket expenses, influencing access to various medical services.
Reimbursement systems contribute to enhancing the efficiency and equilibrium of cost and quality of care within the healthcare industry.
Factors Affecting Reimbursement Rates
Reimbursement rates are influenced by the expenses incurred, the items eligible for reimbursement, potential overpayment issues, and security concerns within the banking industry. Understanding these aspects is crucial for accurate reimbursement calculations.
The key factors that can impact reimbursement rates include:
- Out-of-pocket expenses, which have a direct impact on the financial well-being of account holders.
- Fraud prevention, a critical factor in ensuring transaction integrity and preventing unauthorized transactions.
- Account holder identity verification, essential for minimizing identity theft and ensuring reimbursements reach the intended recipients.
Proactive engagement with these factors can enable financial institutions to build trust, mitigate risks, and streamline the reimbursement process for customers and stakeholders.
Key Variables to Consider
The type of expenses, purpose of travel, organizational policies, legitimate reasons for reimbursement, and fraud prevention are crucial variables in determining reimbursement rates. These variables greatly influence the accuracy and fairness of reimbursement rates.
Ensuring that expenses are directly linked to the business purpose of a trip is a key factor in determining the legitimacy of reimbursement. Fraud prevention measures, such as verifying receipts and conducting regular audits, play a significant role in upholding the integrity of reimbursement processes.
Variables pertaining to organizational policies, such as adherence to guidelines and regular auditing, are essential for maintaining the accuracy and fairness of the reimbursement process. Compliance with organizational policy not only expedites reimbursement but also enhances transparency and accountability in the process.
Aligning reimbursement policies with the organization’s goals fosters a culture of compliance and ethical behavior.
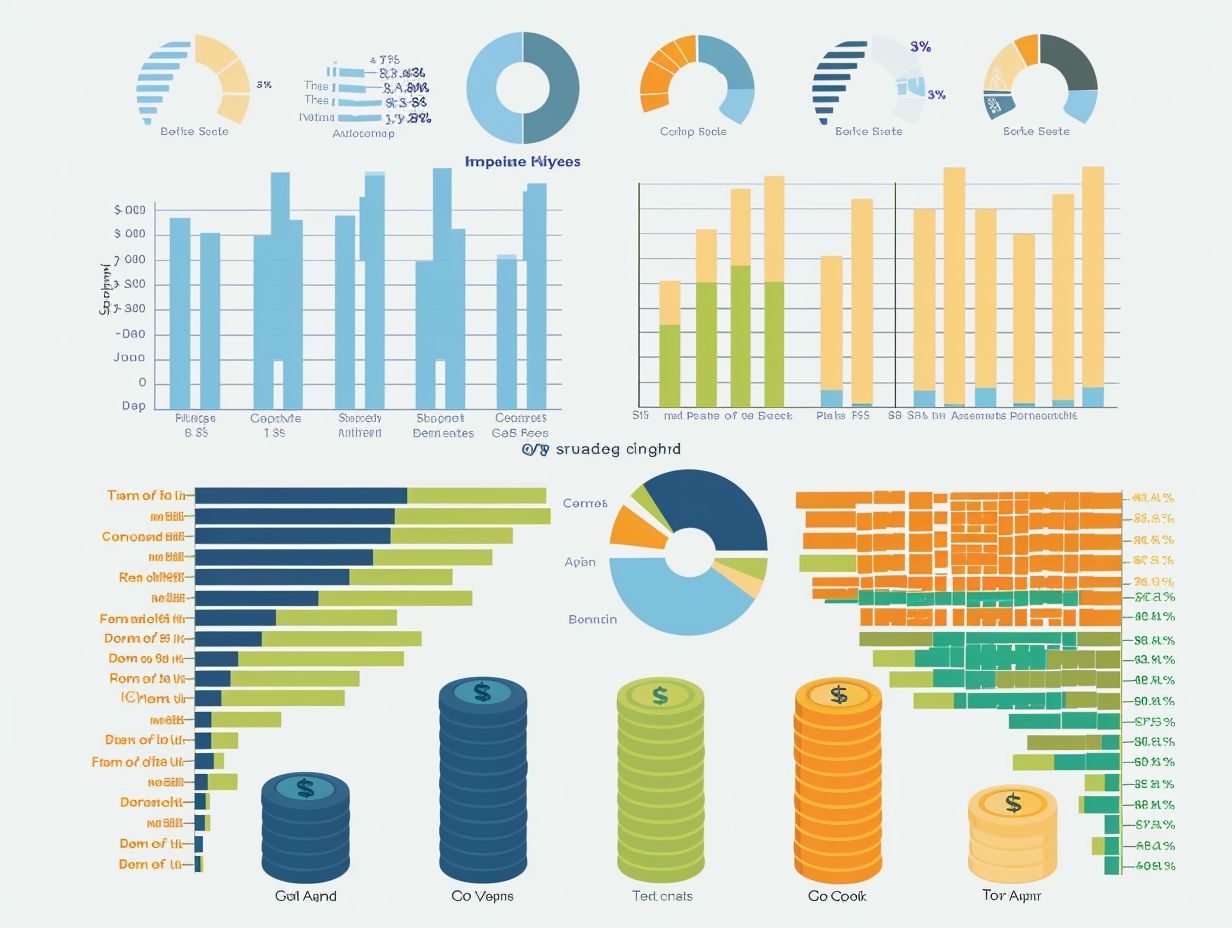
Calculating Reimbursement Rates

- Types of Expenses: Reimbursement rates are determined based on charges, fees, or relative value units (RVUs) for the specific service, depending on the insurer.
- Insurance Policy Terms: The coverage, co-pays, deductibles, and benefit limits outlined in the insurance policy dictate how reimbursement rates are calculated.
- Healthcare Provider Services: The pricing set by healthcare providers plays a key role in determining reimbursement rates.
- Individual Out-of-Pocket Expenses: Reimbursement rates are impacted by the out-of-pocket expenses that patients incur. Patients may need to pay a certain amount out of pocket for services as per the policy, which will then be reimbursed.
Methods and Formulas
- Tax considerations: Federal tax guidelines play a crucial role in determining healthcare providers’ reimbursement amounts. It is essential to understand these guidelines to accurately calculate reimbursement rates and adhere to federal tax laws.
- Health insurance coverage: The terms of medical services provided and the details of the insurance policy significantly impact the specific terms of health insurance policies and the compensation received by healthcare providers. This, in turn, affects the financial outcomes for both healthcare providers and insurance companies. It is imperative to analyze these variables carefully to ensure appropriate reimbursement rates for all stakeholders.
Types of Reimbursement Rates
Reimbursement rates are determined by the type of reimbursement model utilized, with the most common being Fee-for-Service and Capitation models. Different reimbursement structures hold significance for both providers and recipients of reimbursement.
In the Fee-for-Service model, providers are reimbursed for each service they deliver, which is often linked to increased service utilization and the potential overuse of unnecessary services. On the other hand, in the Capitation model, providers receive a fixed, per-member-per-month fee regardless of the services rendered, leading to enhanced healthcare access and quality of care.
The Fee-for-Service model correlates more services provided with higher reimbursement, while the Capitation model offers a consistent payment irrespective of the service provided. Although Capitation entails a lower reimbursement rate, it promotes cost-efficient practices and encourages providers to deliver essential care within the confines of the fixed reimbursement framework.
Fee-for-Service vs. Capitation
There are two major reimbursement models that corporations, employees, and healthcare providers encounter: Fee-for-Service and Capitation. Fee-for-Service involves reimbursement based on the amount of care received, while Capitation entails a set payment per patient regardless of the care utilized.
From a corporate perspective, Fee-for-Service can result in unpredictable costs based on service levels, whereas Capitation offers more predictable budgeting due to its fixed per capita payment structure. Employees may have a broader range of care options with Fee-for-Service, while Capitation may encourage preventive care to effectively manage costs.
Healthcare providers may prefer Fee-for-Service for the potential of higher revenue per service, although Capitation may incentivize a focus on preventive care and overall health. The federal tax implications differ between these models, impacting how corporations handle revenue and expenses related to healthcare services.
Negotiating Reimbursement Rates
Negotiating reimbursement rates is essential for healthcare providers to ensure they are fairly compensated for their services. Effective negotiation strategies are crucial in securing reimbursement rates that enable providers to cover their expenses and meet insurance requirements.
The financial sustainability of healthcare practices is significantly influenced by these negotiations, as reimbursement rates directly impact the revenue they receive. Providers engage in negotiations with insurance companies to establish agreements that are mutually beneficial and accurately reflect the value of the services rendered.
Training in coding, billing practices, and reimbursement methodologies equips healthcare professionals with the knowledge needed to negotiate favorable rates. Successful negotiation tactics in the healthcare reimbursement sector often involve open communication and providing data on the costs associated with delivering quality care.
Tips and Strategies for Providers

Healthcare providers can enhance their success rate in negotiating reimbursement rates with insurance companies by implementing various tips and strategies. These strategies include articulating legitimate reasons for reimbursement, preventing fraud, and accurately documenting incurred expenses.
One highly effective approach is for providers to assess their billing and coding practices to ensure compliance with insurance company guidelines and accuracy. Establishing a system to track and document all patient services can enhance reimbursement efforts.
Staying updated on current regulations and industry changes give the power tos providers to negotiate from a knowledgeable standpoint. Building strong relationships with insurance company representatives is crucial for fostering open communication and resolving disputes effectively.
Maximizing Reimbursement Rates
Maximizing reimbursement rates is achieved through effective billing and coding practices that ensure proper documentation and submission of all legitimate business expenses, including business travel, for reimbursement. Organizations enhance their reimbursement potential by focusing on compliance and operational efficiency.
The process starts with thorough record-keeping of expenses, which not only helps maximize legitimate reimbursement but also ensures compliance with industry regulations. Implementing internal controls and conducting regular audits can assist in detecting discrepancies or instances of fraud.
By adopting these best practices, organizations establish a strong foundation for efficient billing and coding operations, ultimately resulting in higher reimbursement rates.
Optimizing Billing and Coding Practices
Optimizing billing and coding practices is crucial for achieving high reimbursement rates and preventing fraud. By adhering to strong coding protocols, the meticulous documentation of out-of-pocket and business trip expenses can be enhanced to expedite the reimbursement process and reduce errors.
Accurate documentation and categorization of all expenses according to industry standards are essential to avoid costly mistakes that may result in revenue loss. Proper expense categorization not only streamlines the reimbursement process but also enhances the transparency of an organization’s financial records.
Improved fraud detection within coding practices ensures compliance with regulatory requirements and upholds the integrity of the organization’s financial activities. Implementing best practices for coding expenses, such as utilizing advanced software systems and regularly updating coding guidelines, is vital for optimizing billing efficiency.
Frequently Asked Questions
What are reimbursement rates?
Reimbursement rates refer to the amount of money that will be paid back to you for an eligible expense. This is typically a percentage of the total cost, and can vary depending on your insurance plan or employer’s reimbursement policy.
How are reimbursement rates determined?

Reimbursement rates are determined by your insurance provider or employer, based on their specific policies and guidelines. These rates can vary based on the type of expense, location, and other factors.
What expenses are typically covered by reimbursement rates?
Reimbursement rates can cover a variety of eligible expenses, such as medical bills, prescription medications, travel expenses, and more. It is important to check with your insurance provider or employer to understand what expenses are covered under your specific plan.
Do reimbursement rates differ between insurance plans?
Yes, reimbursement rates can vary greatly between different insurance plans. It is important to review your plan’s details to understand the specific reimbursement rates that apply to your plan.
Will I always get the full amount back through reimbursement rates?
No, reimbursement rates may only cover a portion of the total cost of an eligible expense. It is important to check with your insurance provider or employer to understand the specific reimbursement rates that apply to your plan, and if there are any limitations or maximum amounts for certain expenses.
Can reimbursement rates change over time?
Yes, reimbursement rates can change over time. This can be due to changes in your insurance plan or employer’s policies, changes in healthcare costs, or other factors. It is important to regularly review your plan’s details and stay informed about any changes that may affect your reimbursement rates.